Airway Protection in Children With Dysphagia: A Preliminary Study
Copyright 2023 ⓒ Korean Speech-Language & Hearing Association.
This is an Open-Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
The physiology and pathophysiology of pediatric swallowing are challenging due to anatomical differences. There are only a few videofluoroscopic case studies examining the relationship between physiologic events and aspiration in infants, especially, airway protection mechanisms using temporal measurements. This study examined the airway protection mechanisms using two temporal measurements: the initiation and duration of laryngeal closure between two groups of children who were referred for dysphagia evaluation.
Twelve children (8 younger and 4 older children) were patriciate in the study. Initiation of laryngeal closure (ILC) and laryngeal closure duration (LCD) were measured using videofluoroscopic swallowing examinations (VFSEs) with a 100-ms timer for bottle-fed or 2mL thin liquids and/or puree boluses. Two-way analysis of variance (ANOVA) was used at a significance level of p<.05.
Younger children showed longer LCD than older children. There was no significant difference in ILC between younger and older children with dysphagia. The puree had longer ILC and shorter LCD than the thin liquid bolus.
The longer duration of laryngeal closure in younger children may indicate that their anatomical structure is more prone to better protect their airways than older children. Longer ILC and shorter LCD were observed in both children groups who presented penetration or aspiration. These pathophysiological phenomena should be observed closely as indicators of the higher risk of dysphagia. Bolus modification such as thickened liquid may help the children to keep from aspiration.
Keywords:
Laryngeal closure, airway protection, pediatric, swallowing, aspirationⅠ. Introduction
During normal swallowing, food and liquid are safely and efficiently transported from the mouth to the stomach. Babies who are developmentally immature or medically frail may have trouble feeding and swallowing; therefore, they may fail to thrive and/or experience malnutrition, dehydration and/or respiratory distress (Lefton-Greif, 2008). Because babies are physiologically immature, their feeding/swallowing behaviors are distinctively different from adults. Normally, babies reflexively coordinate sucking, breathing, and swallowing (Mizuno et al., 2007). In fragile infants, poor coordination or fatigue may lead to negative swallowing experiences, inadequate intake, or refusal of oral intake. These infants may also show excessive gagging or recurrent cough during feeding, weight loss or lack of weight gain for 2~3 months, and prolonged feeding times (>30~40minutes) (Lau et al., 2000; Loughlin, 1989; Medoff-Cooper et al., 2002). Consequently, swallowing disorders in the pediatric population are an issue of survival and development. The pediatric population with dysphagia often shows misdirection of bolus during the swallow, which may be related to the occurrence of aspiration.
Swallowing can be divided into three physiologic stages: oral, pharyngeal, and esophageal (Logemann, 1998). One of the pathophysiological characteristics during oral and pharyngeal transition is the slow onset of the laryngeal closure and/or early reopening of laryngeal closure. The researchers have focused on airway protection in adults with dysphagia using analyzing videofluoroscopic swallowing examination (VFSE) (Logemann et al., 1992; Park et al., 2010), however, it is hard to apply the physiology and pathophysiology of adult swallowing to the pediatric population. This approach allows direct observation of the extent of airway protection during swallowing, e.g., laryngeal closure duration (LCD) measures the duration of contact between two critical structures in the laryngo-pharynx, the epiglottis and arytenoids (Park et al., 2010). In addition, this approach allows direct observation of the bolus as it moves from the mouth into the pharynx, e.g., one temporal measure, initiation of laryngeal closure (ILC) pinpoints the starting point of swallowing relative to the position of the bolus to determine whether the pharyngeal swallow is delayed. The outcomes of this study guide clinicians in their choice of therapy, e.g., when an infant aspirates because the pharyngeal swallow is delayed, bolus consistency/viscosity can be modified to compensate for the delay (Lustre et al., 2013).
Unfortunately, there are only a few videofluoroscopic case studies examining the relationship between physiologic events and aspiration in infants (Arvedson & Lefton-Geif, 2017; Flax-Goldenberg et al., 2016; Weckmueller et al., 2011). The current study focused on examining swallowing physiology and pathophysiology of airway closure in bottle-fed infants using temporal measures. The purpose of this study was to examine the pathophysiology of laryngeal closure in pediatric populations with dysphagia. This study is preliminary in nature to develop a diagnostic protocol for infants and children who are at risk of swallowing disorders.
Ⅱ. Methods
1. Subjects and Experimental Procedures
8 younger and 4 older children who were referred to the videofluoroscopic swallowing examination (VFSE) were included. The subjects were divided into two separate age groups. Among them, 8 children between the of .5 and 4.2 years were included in the younger children group, and 4 children between the ages of 8 and 9.11 years were included in the older children group. Demographic information of the participating children was presented at Table 1.
The VFSE was gathered after the referral from pediatricians at the tertiary hospital in Korea. The VFSE procedure was as follows: Each child sat on the tumble form feeder seat in the fluorographic suite. Children were fed by way of bottle or spoon. Spoon fed children had 2mL thin liquids and/or puree boluses. Lateral view of x-ray videoclips were submitted for analysis.
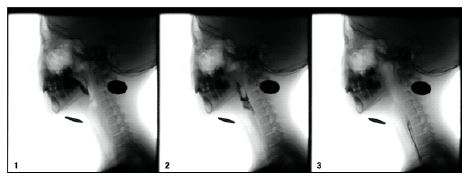
To analyze the initiation and duration of laryngeal closure in VFSE videoclips, three points were documented on each subject: (1) bolus passing the ramus of the mandible, (2) the first contact of the arytenoids and epiglottis, and (3) the last moment of contact between the arytenoids and epiglottis (Kendall et al., 2004; Perlman et al., 1994). Initiation of laryngeal closure (ILC) was calculated by subtracting the point of contact with the arytenoids and epiglottis from the time the bolus passed the ramus of the mandible. The laryngeal closure duration (LCD) was measured by subtracting the last point of contact of the arytenoids and the epiglottis from the first point of contact. Figure 1. Two-way analysis of variance (ANOVA) of group and consistency comparison as independent variables were used at p<.05.
Ⅲ. Results
1. Reliability
For intra-judge reliability, the investigator randomly selected and reanalyzed 20% of the subjects. A significant correlation between the first and second judgment was observed for initiation (r=.94, p<.01) and duration of laryngeal closure (r=.98, p<.01). For inter-judge reliability, a second judge analyzed the same subjects. That judge’s results were compared with the results of the primary investigator. A significant correlation was observed between judges for initiation (r=.98, p<.01) and duration of laryngeal closure (r=.96, p<.01).
2. Occurrence of Penetration and Aspiration
For the occurrence of penetration and aspiration, two children (one younger and one older) showed aspiration and seven (five younger and two older children) showed penetration in thin liquid only.
3. Initiation of Laryngeal Closure (ILC)
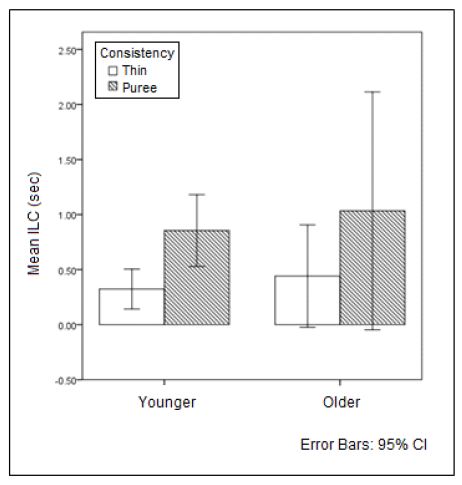
There was no difference in the initiation of laryngeal closure (ILC) between the younger and older children (F(1, 50)=.44, p=.51). The mean ILC in the younger children was approximately .59 seconds and .74 seconds in the older children. The ILC in the puree was significantly longer than the ILC for the thin liquid (F(1, 50)=6.35, p=.02). The mean ILC of the thin liquid was .95 seconds and of the puree was .38 seconds (Figure 2).
4. Laryngeal Closure Duration (LCD)
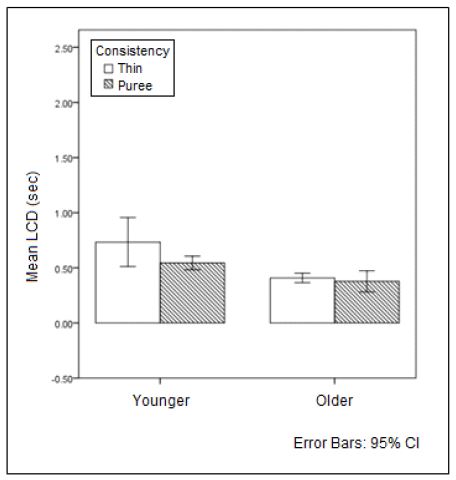
Laryngeal closure duration (LCD) was significantly different between the younger and older children (F(1, 34)=20.58, p<.001). The mean LCD of the younger children was .64 seconds, and the mean LCD of older children was .40 seconds. Younger children showed longer laryngeal closure duration than older children. The LCD in the puree was significantly longer than the LCD for the thin liquid (F(1, 34)=4.13, p=.048). The mean LCD of the thin liquid was 0.36 seconds, and LCD of the puree was .94 seconds (Figure 3).
Ⅳ. Discussion
This study found that the ILC did not differ between younger and older children. This finding may indicate that the initiation of laryngeal closure in the pediatric population is executed reflexively regardless of age. In addition, initiation of laryngeal closure in thin liquid was quickly initiated than in puree. The transition of thin liquid is faster than puree (Kim et al., 2021), so quick ILC is necessary to prevent entering the bolus prior to complete closure of the larynx during the thin liquid swallow.
Younger children had longer LCD than older children since ILC was not different between younger and older children. LCD and ILC were significantly different between thin and puree consistencies. Longer laryngeal closure duration may be related to differences in anatomical development. The larynx in younger children is located at a higher position (Vorperian et al., 2009). The higher position of the larynx in younger children may help maintain the laryngeal closure for a sufficient period. Furthermore, a longer duration of laryngeal closure may be necessary to compromise not fully matured laryngeal structures. True vocal folds are the important valve for airway protection, but younger children do not have a distinct layer of vocal folds and not developed vocal ligaments before 4 years of age (Zemlin, 1998). A longer duration of laryngeal closure supports other immature laryngeal structures of the airway during the swallow. LCD in thin liquid was longer than puree. This may be related to the consistency characteristic that thin liquid is less cohesive than puree and is easily spread during the transition. The longer LCD in thin liquid may be more beneficial to facilitating a safe swallow than in puree.
The current study showed that there is an interesting relationship between initiation/duration of laryngeal closure and swallowing physiology. In general, longer ILC and shorter LCD were observed in children who presented penetration or aspiration. These pathophysiological phenomena should be observed closely as indicators of the higher risk of dysphagia. However, when subject number 12, an older child, swallowed puree six times, her ILC was over 2 seconds but did not show aspiration or penetration. She did not let the bolus move to the vallecula to swallow until all the bolus was collected and ready to swallow as a whole in the oral cavity. She may develop a strategy to swallow safely in case of long delays of pharyngeal swallowing. It is important to have posterior tongue strength and maintain anterior faucial pillar and tongue closure for preventing the bolus from entering the pharynx. What is the proper capacity of the bolus to hold in the oral cavity? Individual swallowing capacity of the bolus held in the oral cavity should be studied. On the other hand, different from adults, pediatric populations have a beneficial mechanism in the sensory aspects of swallowing. The children squeeze the nipple, which stimulates the anterior faucial pillar every swallow. It may help the children to be more sensitive to bolus amount and capable of recognizing the threshold to hold the bolus effectively in the oral cavity.
Those who aspirated showed longer ILC and shorter LCD than those without aspiration, in general. However, subject 11, an older child, showed different swallowing patterns between thin liquid and puree consistencies. In thin liquid, his ILC was over 1 second and his LCD was less than 1 second. In the puree, his ILC was over 2 seconds, and his LCD also was over 2 seconds. He showed aspiration in thin liquid but did not in the puree. Consistency should be considered to analyze the airway protection mechanism. Puree showed longer delay than thin liquid but longer LCD in puree may compensate for physiological difficulty from the delayed pharyngeal swallow. The findings of this study are similar to Park et al. (2010) in adults longer LCD in puree may keep the patients from experiencing aspiration or penetration than other consistencies.
Temporal measurements of adult swallowing have been shown to be reliable tools for describing normal swallowing functions (Robbins et al., 1992; Robbins, 1996; Logemann et al., 2000, Logemann, 2002). In addition, these measurements enhance the efficacy of swallowing treatment strategies through an improved evidence base. The indicators of aspiration risk could be studied using temporal measurements, which will help clinicians establish temporally valid treatment strategies and follow-up plans based on the risk of aspiration. Temporal measurements of pediatric populations with normal or abnormal swallowing were extremely limited. This study showed that there is good potential to apply temporal measures to pediatric populations with dysphagia to understand swallowing physiology and pathophysiology such as delayed pharyngeal swallowing and airway protection. The temporal measurements are also able to help to choose specific compensatory or rehabilitation strategies to improve swallowing function in children. More studies is needed regarding compensating and rehabilitating swallowing functions specific to the occurrence of aspiration.
V. Conclusion
The findings in this study support understanding the physiology and pathophysiology of airway protection in the pediatric population with dysphagia. Thickening liquid and bolus modification will influence the safety of swallowing. As a pediatric clinician, it is important to find and recommend appropriate treatment or management strategies based on VFSE results in pediatric populations. There are several limitations of this study such as a small number of subjects and heterogeneous groups. Future studies should include a large number of subjects and homogenous groups.
Acknowledgments
This study did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
References
-
Arvedson, J. C., & Lefton-Greif, M. A. (2017). Instrumental assessment of pediatric dysphagia. Seminars in Speech and Language, 38(2), 135-146.
[https://doi.org/10.1055/s-0037-1599111]

-
Lustre, N. S., Freire, T. R. B., & Silverio, C. C. (2013). Temporal measurements of oral transit time in children with cerebral palsy of different levels motors and the relationship with the severity of dysphagia. Audiology-Communication Research, 18(3), 155-161.
[https://doi.org/10.1590/S2317-64312013000300004]

-
Flax-Goldenberg, R., Kulkarni, K. S., Carson, K. A., Pinto, J. M., Martin-Harris, B., & Lefton-Greif, M. A. (2016). Concordance between aspiration detected on upper gastrointestinal series and videofluoroscopic swallow study in bottle-fed children. Dysphagia, 31(4), 505-510.
[https://doi.org/10.1007/s00455-016-9705-y]

-
Kendall, K. A., Leonard, R. J., & McKenzie, S. (2004). Airway protection: Evaluation with videofluoroscopy. Dysphagia, 19(2), 65–70.
[https://doi.org/10.1007/s00455-003-0500-1]

-
Kim, Y., Williams, B., Park, T., Oommen, E., & McCullough, G. H. (2021). Effect of age, gender, and consistency in normal swallowing. Journal of Speech, Language & Hearing Disorders, 30(2), 69-75.
[https://doi.org/10.15724/jslhd.2021.30.2.069]

-
Lau, L., Alagugurusamy, R., Shulman, R. J., Smith, E. I., & Schanler, R. J. (2000). Characterization of the developmental stages of sucking in preterm infants during bottle feeding. Acta Paediatrica, 89(7), 846-852.
[https://doi.org/10.1111/j.1651-2227.2000.tb00393.x]

-
Lefton-Greif, M. A. (2008). Pediatric dysphagia. Physical Medicine and Rehabilitation Clinics of North America, 19(4), 837-851.
[https://doi.org/10.1016/j.pmr.2008.05.007]

-
Logemann, J. A. (1998). Evaluation and treatment of swallowing disorders. Austin:Pro:ed.
[https://doi.org/10.1097/00020840-199812000-00008]

-
Logemann, J. A., Kahrilas, P. J., Cheng, J. O. A. N., Pauloski, B. R., Gibbons, P. J., Rademaker, A. W., & Lin, S. H. E. Z. H. A. N. G. (1992). Closure mechanisms of laryngeal closure during swallow. American Journal of Physiology, Gastrointestinal and Liver Physiology, 262(2), G338-G344.
[https://doi.org/10.1152/ajpgi.1992.262.2.G338]

-
Logemann, J. A., Pauloski, B. R., Rademaker, A. W., Colangelo, L. A., Kahrilas, P. J., & Smith, C. H. (2000). Temporal and biomechanical characteristics of oropharyngeal swallow in younger and older men. Journal of Speech, Language, and Hearing Research, 43(5), 1264-1274.
[https://doi.org/10.1044/jslhr.4305.1264]

-
Logemann, J. A., Pauloski, B. R., Rademaker, A. W., & Kahrilas, P. J. (2002). Oropharyngeal swallow in younger and older women: videofluoroscopic analysis. Journal of Speech, Language, and Hearing Research, 45(3), 434-445.
[https://doi.org/10.1044/1092-4388(2002/034)]

-
Loughlin, G. M. (1989). Respiratory consequences of dysfunctional swallowing and aspiration. Dysphagia, 3(3), 126-130.
[https://doi.org/10.1007/BF02407130]

-
Medoff-Cooper, B., McGrath, J. M., & Shults, J. (2002). Feeding patterns of full-term and preterm infants at forty weeks postconceptional age. Journal of Developmental and Behavioral Pediatrics, 23(4), 231-236.
[https://doi.org/10.1097/00004703-200208000-00007]

-
Mizuno, K., Nishida, Y., Taki, M., Hibino, S., Nurase, M., Sakurai, M., & Itabashi, K. (2007). Infants with bronchopulmonary dysplasia suckle with weak pressures to maintain breathing during feeding. Pediatrics, 120(4), 21035-e1042.
[https://doi.org/10.1542/peds.2006-3567]

-
Park, T., Kim, Y., Ko, D. H., & McCullough, G. H. (2010). Initiation and duration of laryngeal closure during the pharyngeal swallow in post-stroke patients. Dysphagia, 25(3), 177-182.
[https://doi.org/10.1007/s00455-009-9237-9]

-
Perlman, A. L., Booth, B. M., & Grayhack, J. P. (1994). Videofluoroscopic predictors of aspiration in patients with oropharyngeal dysphagia. Dysphagia, 9, 90-95.
[https://doi.org/10.1007/BF00714593]

-
Robbins, J. A., Hamilton, J. W., Lof, G. L. & Kempster, G. B. (1992). Oropharyngeal swallowing in normal adults of different ages. Gastroenterology, 103(3), 823–829.
[https://doi.org/10.1016/0016-5085(92)90013-O]

-
Robbins, J. A. (1996). Normal swallowing and aging. In seminars in Neurology, 16(4), 309-317.
[https://doi.org/10.1055/s-2008-1040989]

-
Weckmueller, J., Easterling, C., & Arvedson, J. (2011). Preliminary temporal measurement analysis of normal oropharyngeal swallowing in infants and young children. Dysphagia, 26(2), 135-143.
[https://doi.org/10.1007/s00455-010-9283-3]

-
Vorperian, H., Wang, S., Chung, M. K., Schimek, E. D., Durtschi, R. B., & Ket, R. D. (2009). Anatomic development of the oral and pharyngeal portions of the vocal tract: An imaging study. Journal of the Acoustical Society of America, 125, 1666-1678.
[https://doi.org/10.1121/1.3075589]

- Zemlin, W. (1998). Speech and hearing science: Anatomy and physiology. Boston: Allyn & Bacon.